Damiano Ricci MD, Guido Grappiolo MD,
Matthew Franco BA, Federico Della Rocca MD
Abstract
Background Osteoid osteomas consist of a nidus surrounded by reactive sclerotic bone. The diagnosis typically is based on imaging and clinical presentation involving nocturnal pain. Removal of the lesion is essential and currently is performed mainly with image-guided, minimally invasive techniques. We describe a case involving an osteoid osteoma of the acetabular fossa, treated with arthroscopy-assisted radiofrequency ablation.
Case Description A 47-year-old woman presented with a 9-month history of right groin pain and limited motion. The CT and MR images showed synovitis around the ligamentum teres and a nidus of the acetabular fossa, surrounded by sclerotic bone and protruding from the inner part of the lamina quadrilateral. Synovectomy and debridement of the ligamentum teres were performed, followed by radiofrequency ablation of the osteoid osteoma under direct arthroscopic observation of the hip, avoiding resection of the normal bone around the nidus and preserving the integrity of the quadrilateral lamina and cartilage. The patient had complete pain relief the next day with minimal morbidity and rapid functional restoration. At the 22-month clinical followup, the patient was asymptomatic, and the CT and MR images obtained 1 year after surgery showed no pathologic signs or synovitis.
Literature Review Our case was the fifth such case to be treated with hip arthroscopy and the first of these to our knowledge to be treated with the arthroscopy-assisted radiofrequency ablation technique.
Purposes and Clinical Relevance Arthroscopy-assisted radiofrequency ablation is a combined treatment technique that may be used for intraarticular lesions of the hip that otherwise would require a difficult approach and jeopardize damage to cartilage and bone and also treat concomitant synovitis.
Introduction
An osteoid osteoma (OO) is a small, benign, osseous neoplasm characterized by a nidus with a maximum growth potential of 1.5 cm, surrounded by reactive sclerotic bone[32]. Osteoid osteomas represent 13% of all benign tumors[68] and typically are associated with nocturnal pain[22]. An OO most commonly occurs between the ages of 5 to 25 years with a male-to-female ratio of 3:1. The subcortical shaft and metaphysis of long bones are the most common lesion sites. The femur and tibia account for greater than 50%; however, lesion sites are ubiquitous[68]. This tumor is rare in the pelvis (range, 2.3%–3.0%)[7,13].
An OO diagnosis can be confirmed with a combination of plain radiographs, technetium-99m (Tc-99m) bone scans, CT scans, and MR images. Plain radiographs can detect an oval, radiolucent, central nidus with a surrounding dense, reactive sclerosis mass, specifically for cortical lesions[31]. Detection is difficult for intramedullary lesions or locations on the spine, pelvis, hands, or feet[17]. Tc-99m bone scans are sensitive for detecting areas with increased activity of osteoblasts, allowing for localization of the lesion[8]. CT scans are the best imaging technique for observing the nidus in cortical and subperiosteal OOs, especially in complex anatomic sites (eg, the pelvis and spine) and when differentiating between several bone neoplasms[16]. MRI, specifically, dynamic gadoliniumenhanced MRI, is useful for diagnosing conditions located in atypical locations, such as trabecular and intraarticular osteomas[34,67,72].
An OO is characterized by local pain that is more frequent and severe at night. NSAIDS or salicylates are justifiable nonsurgical treatments[42]. For cases of severe pain with little to no response to pharmacologic treatment, an operative treatment is recommended. Removal is necessary for juxtaarticular and intraarticular lesions in young patients to prevent developmental complications, such as growth disturbances[25]. The CT-guided radiofrequency ablation (RFA) is a minimally invasive technique and considered the preferred treatment owing to a 91% success rate and low complications compared with an open surgical procedure[59]. This procedure is challenging, being near neurologic structures and juxtaarticular and intraarticular localizations[2,53].
We describe the case of a patient with OO of the acetabulum treated by RFA performed under arthroscopic control to treat concomitant synovitis.
Case Report
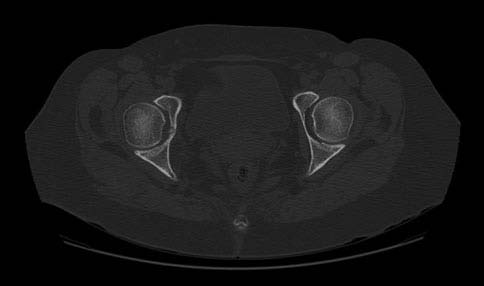
A 47-year-old woman presented with a 9-month history of right groin and anterior thigh pain without injury. The pain intensified at night and was only partially alleviated by NSAIDs and analgesics. On physical examination, she limped with an antalgic gait and had limited ROM of her hip, with 0° to 100° flexion and 0° internal rotation. The pelvic, hip, and lumbar spine radiographs were normal. A CT scan showed an oval, lytic lesion with a 6-mm central nidus at the bottom of the acetabulum with expansion of the quadrilateral plate from the pelvis (Fig. 1). MR images showed an intraarticular lesion with substantial increased signal intensity of the cancellous bone around the acetabulum and concomitant increased signal intensity of the belly of the internal obturator muscle (Fig. 2).
RFA was performed during the arthroscopic procedure while the patient was under general anesthesia and in the supine position. Traction was maintained by a specialized extension room table, using an extra-wide and padded perineal post. An image intensifier was used to confirm the amount of traction, facilitate portal placement, and control the location of the electrode during the procedure (Fig. 3). The standard anterolateral and midanterior portals were established for use of the 70°-arthroscope. We observed no cartilage damage of the hip but severe synovial proliferation was noted around the ligamentum teres (Fig. 3 A). Synovectomy and debridement of the ligamentum teres were performed (Fig. 3 B). A rigid radiofrequency electrode with a diameter of 1 mm then was inserted through a cannula without normal saline inflow to reach the temperature (Fig. 3 C). The lesion then was heated to 90°C for 7 minutes under arthroscopic and image intensifier control, avoiding a resection of the normal bone around the nidus and preserving the integrity of the quadrilateral lamina and cartilage (Fig. 3 D). The surgical time was 85 minutes. A histologic examination was not performed.

The patient had complete pain relief the following day. Low molecular weight heparin and antiembolism stockings were used postoperatively for 15 days and 3 weeks, respectively. Weightbearing was partially limited by the use of two crutches for 2 weeks. At the 22-month followup, the patient had no pain, a normal gait, and normal ROM, and the CT scan (Fig. 4) and MR images at 1 year showed no pathologic signs or synovitis. The patient agreed that information concerning this case could be published.


Discussion
Cortical bone (80%) is the most common lesion site for OO; intramedullary and trabecular sites are less common,
ligamentum teres were performed; (C) the lesion being heated to 90°C for 7 minutes using a rigid radiofrequency electrode with a diameter of 1 mm; and (D) the lesion after ablation of the nidus.
and subperiosteal is rare [13,68]. The acetabulum is an uncommon but painful location often associated with children[29]. There have been numerous reported cases of OO in the acetabulum [4,9,18,20,21,28,29,36,40,41,44,48,49,52,55,56,67].
Juxtaarticular and intraarticular localizations frequently are associated with a delayed diagnosis, as seen in our patient[24].
Cases of spontaneous healing of OO treated with NSAIDs have been reported[35,42], but regression may be lengthy (up to 36 months)[30] and delayed treatment of intraarticular cases can damage the articulation[3,15,66] and cause early osteoarthritis[23,54].
Numerous open surgical techniques involving removal of benign tumors in the pelvis have been described[12,20,51]. The rate of recurrence with surgical therapy ranges from 0% to 12% in published series[13,58,64,70,71]. Disadvantages of these approaches include activity restrictions if the tumor was in a weightbearing location[70], the need for plating in some patients[13,64], donor site morbidity if grafting is used[71], and postoperative fracture[64].
Some authors suggest complete removal of the nidus is mandatory, leaving the thickened bone around the OO[13,68]. CT-guided percutaneous resection has been commonly used for the past decade, especially for difficult locations like the acetabulum[43,56,62]. Other percutaneous techniques have been proposed, such as laser thermal therapy, cryotherapy, and ethanol therapy[1,2,26,27].
CT-guided RFA has become the preferred method owing to a low morbidity rate, minimal postoperative complications, minimal tissue exposure, rapid recovery, and no restriction of weightbearing activity [10,14,33,50,60,69].
In addition, the healing rate is 76% to 100%[14,53], with a major complication rate of 0% to 5%[2,6,45]. However, using CT-guided RFA, there are reports of articular cartilage damage in weightbearing joints; one patient experienced articular cartilage damage to the talus[47], and another had damage to the acetabulum[9]. Direct observation and femoral head distraction during the arthroscopy may decrease the risk of cartilaginous thermal damage.
Treatment of intraarticular hip lesions with CT-guided RFA is challenging, and caution is required in this situation[55]. We believe that a concerning interruption of subchondral bone continuity is unavoidable using percutaneous methods when reaching the central articular zone of the acetabulum because of the thin bone and the proximity to the joint.
Hip arthroscopy has become popular during the last decade with a widespread expanding list of indications, such as septic arthritis, loose body, labral tears, extraar ticular lesions, and femoroacetabular impingement[5,38,39,46,57,65]. However, this approach, like the others mentioned, has limitations. To minimize the risk of nerve injury[11,19], it is necessary to not exceed 50 pounds and 90 minutes of continuous traction; otherwise, traction is temporarily released[61,63]. In addition, not all areas of the acetabulum are easy to access; the inferior area of the acetabulum is almost inaccessible with arthroscopy, even when using a flexible probe. Synovitis is common with intraarticular tumor locations; it appears to depend on the release of cyclooxygenase-2 by osteoblasts of the nidus[37]. Synovectomy can be done during lesion removal, which may prevent cartilage damage, speed the healing process, and relieve pain immediately[15,28,44].
We found descriptions of four cases using arthroscopic excision of the OO of the acetabulum. Three were located in the acetabular fossa of adult patients[4,18,40]. In two patients[4,40] the OO was located in the posterior area and the other[18] was in the posteroinferior area which was more difficult to reach. In the fourth patient (a 10-yearold boy)[44], the lesion was located under the triradiate cartilage. Our patient is the first to our knowledge treated with an arthroscopic-assisted RFA technique. No recurrences have been reported in these five cases.
We used arthroscopy for debridement and synovectomy to minimize the risk of damage to the articular cartilage with the use of percutaneous RFA and avoid disruption of the medial wall bone with the use of the arthroscopic burr, with no clinical recurrence at 22 months of followup.
References
- Adam G, Neuerburg J, Vorwerk D, Forst J, Gunther RW. Per cutaneous treatment of osteoid osteomas: combination of drill biopsy and subsequent ethanol injection. Semin Musculoskelet Radiol. 1997;1:281–284.
- Akhlaghpoor S, Aziz Ahari A, Arjmand Shabestari A, Alinaghizadeh MR. Radiofrequency ablation of osteoid osteoma in atypical locations: a case series. Clin Orthop Relat Res. 2010;468:1963–1970.
- Alani WO, Bartal E. Osteoid osteoma of the femoral neck stimulating an infiammatory synovitis. Clin Orthop Relat Res. 1987;223:308–312.
- Alvarez MS, Moneo PR, Palacios JA. Arthroscopic extirpation of an osteoid osteoma of the acetabulum. Arthroscopy. 2001;17: 768–771.
- Awan N, Murray P. Role of hip arthroscopy in the diagnosis and treatment of joint pathology. Arthroscopy. 2006;22:215–218.
- Barei DP, Moreau G, Scarborough MT, Neel MD. Percutaneous radiofrequency ablation of osteoid osteoma. Clin Orthop Relat Res. 2000;373:115–124.
- Bettelli G, Capanna R, Vanhorn JR, Ruggieri P, Biagini R, Campanacci M. Osteoid osteoma and osteoblastoma of the pelvis. Clin Orthop Relat Res. 1989;247:261–271.
- Blaskiewicz DJ, Sure DR, Hedequist DJ, Emans JB, Grant F, Proctor MR. Osteoid osteoma: Intraoperative bone scan-assisted resection. J Neurosurg Pediatr. 2009;4:237–244.
- Bosschaert PP, Deprez FC. Acetabular osteoid osteoma treated by percutaneous radiofrequency ablation: delayed articular cartilage damage. JBR-BTR. 2010;93:204–206.
- Bruners P, Penzkofer T, Gunther RW, Mahnken A. Percutaneous radiofrequency ablation of osteoid osteomas: technique and results. Rofo. 2009;181:740–747.
- Byrd JW. Hip arthroscopy utilizing the supine position. Arthroscopy. 1994;10:275–280.
- Callaghan JJ, Salvati EA, Pellicci PM, Bansal M, Ghelman B. Evaluation of benign acetabular lesions with excision through the Ludloff approach. Clin Orthop Relat Res. 1988;237:170–178.
- Campanacci M, Ruggieri P, Gasbarrini A, Ferraro A, Campanacci
- L. Osteoid osteoma. Direct visual identification and intralesional excision of the nidus with minimal removal of bone. J Bone Joint Surg Br. 1999;81:814–820.
- Cantwell CP, Obyrne J, Eustace S. Current trends in treatment of osteoid osteoma with an emphasis on radiofrequency ablation. Eur Radiol. 2004;14:607–617.
- Cassar-Pullicino VN, McCall IW, Wan S. Intraarticular osteoid osteoma. Clin Radiol. 1992;45:153–160.
- Cerase A, Priolo F. Skeletal benign bone-forming lesions. Eur J Radiol. 1998;27(suppl 1):S91–S97.
- Chai JW, Hong SH, Choi JY, Koh YH, Lee JW, Choi JA, Kang HS. Radiologic diagnosis of osteoid osteoma: from simple to challenging findings. Radiographics. 2010;30:737–749.
- Chang BK, Ha YC, Lee YK, Hwang DS, Koo KH. Arthroscopic excision of osteoid osteoma in the posteroinferior portion of the acetabulum. Knee Surg Sports Traumatol Arthrosc. 2010;18: 1685–1687.
- Clarke MT, Arora A, Villar RN. Hip arthroscopy: complications in 1054 cases. Clin Orthop Relat Res. 2003;406:84–88.
- Cohen RV. Osteoid osteoma of the acetabulum. Clin Orthop Relat Res. 1994;304:204–206.
- Dejour H, Leclerc P, Nourissat C. Oste´ome oste´oide du fond du cotyle. Rev Chir Orthop Reparatrice Appar Mot. 1975;61:755–758.
- Dockert MB, Ghormley RK, Jackson AE. Osteoid osteoma: clinicopathologic study of 20 cases. Ann Surg. 1951;133:77.
- Foeldvari I, Schmitz MC. Rapid development of severe osteo arthritis associated with osteoid osteoma in a young girl. Clin Rheumatol. 1998;17:534–537.
- Franceschi F, Marinozzi A, Papalia R, Longo UG, Gualdi G, Denaro E. Intra-and juxta-articular osteoid osteoma: a diagnostic challenge: misdiagnosis and successful treatment: a report of four cases. Arch Orthop Trauma Surg. 2006;126:660–667.
- Frassica FJ, Waltrip RL, Sponseller PD, Ma LD, McCarthy EF Jr. Clinicopathologic features and treatment of osteoid osteoma and osteoblastoma in children and adolescents. Orthop Clin North Am. 1996;27:559–574.
- Gangi A, Dietemann JL, Clavert JM, Dodelin A, Mortazavi R, Durckel J, Roy C. Treatment of osteoid osteoma using laser photocoagulation: apropos of 28 cases. Rev Chir Orthop Reparatrice Appar Mot. 1998;84:676–684.
- Ghanem I. The management of osteoid osteoma: updates and controversies. Curr Opin Pediatr. 2006;18:36–41.
- Gille P, Gross P, Brax P, Carcopino JM, Aubert D, Giordan H. Osteoid osteoma of the acetabulum: two cases. J Pediatr Orthop. 1990;10:416–418.
- Goldberg VM, Jacobs B. Osteoid osteoma of the hip in children. Clin Orthop Relat Res. 1975;106:41–47.
- Goto T, Shinoda Y, Okuma T, Ogura K, Tsuda Y, Yamakawa K, Hozumi T. Administration of nonsteroidal anti-inflammatory drugs accelerates spontaneous healing of osteoid osteoma. Arch Orthop Trauma Surg. 2011;131:619–625.
- Greenspan A. Benign bone-forming lesions: osteoma, osteoid osteoma, and osteoblastoma -clinical, imaging, pathologic, and differential consideration. Skeletal Radiol. 1993;22:485–500.
- Healey JH, Ghelman B. Osteoid osteoma and osteoblastoma: current concepts and recent advances. Clin Orthop Relat Res. 1986;204:76–85.
- Hoffmann RT, Jakobs TF, Kubisch CH, Trumm CG, Weber C, Duerr HR, Helmberger TK, Reiser MF. Radiofrequency ablation in the treatment of osteoid osteoma: 5-year experience. Eur J Radiol. 2010;73:374–379.
- Hosalkar HS, Garg S, Moroz L, Pollack A, Dormans JP. The diagnostic accuracy of MRI versus CT imaging for osteoid osteoma in children. Clin Orthop Relat Res. 2005;433:171–177.
- Ilyas I, Young DA. Medical management of osteoid osteoma. Can J Surg. 2002;45:435–437.
- Karray S, Zlitni M, Karray M, Moalla M, Zouari M, Douik M, Sliman N. Osteoid osteoma of the acetabulum. Int Orthop. 1993;17:54–56.
- Kawaguchi Y, Sato C, Hasegawa T, Oka S, Kuwahara H, Nor imatsu H. Intraarticular osteoid osteoma associated with synovitis: a possible role of cyclooxygenase-2 expression by osteoblasts in the nidus. Mod Pathol. 2000;13:1086–1091.
- Kelly BT, Williams RJ, Philippon MJ. Hip arthroscopy: current indications, treatment options, and management issues. Am J Sports Med. 2003;31:1020–1037.
- Khanduja V, Villar RN. Arthroscopic surgery of the hip: current concepts and recent advances. J Bone Joint Surg Br. 2006;88: 1557–1566.
- Khapchik V, O’Donnel RJ, Glick JM. Arthroscopically assisted excision of osteoid osteoma involving the hip. Arthroscopy. 2001;17:56–61.
- Klingenberg L, Konradsen L. [Osteoid osteoma in the hip of 12 year-old girl][in Danish]. Ugeskr Laeger. 2008;170:4142.
- Kneisl JS, Simon MA. Medical management compared with operative treatment for osteoid osteoma. J Bone Joint Surg Am. 1992;74:179–185.
- Kohler R, Rubini J, Postec F, Canterino I, Archimbaud F. Treatment of osteoid osteoma by CT-controlled percutaneous drill resection: apropos of 27 cases. Rev Chir Orthop Reparatrice Appar Mot. 1995;81:317–325.
- Lee DH, Jeong WK, Lee SH. Arthroscopic excision of osteoid osteomas of the hip in children. J Pediatr Orthop. 2009;29:547–
- 551.
- Lindner NJ, Ozaki T, Roedl R, Gosheger G, Winkelman W, Wortler K. Percutaneous radiofrequency ablation in osteoid osteoma. J Bone Joint Surg Br. 2001;83:391–396.
- Lubowitz JH. Hip arthroscopy: an emerging gold standard. Arthroscopy. 2006;22:1257–1259.
- Migues A, Velan O, Solari G, Pace G, Slullitel G, Araujo ES. Osteoid osteoma of the calcaneus: percutaneous radiofrequency ablation. J Foot Ankle Surg. 2005;44:469–472.
- Miller SJ, Smith DW, Beckett WW, Gaines RW. Intra-articular osteoid osteoma of the acetabulum in a 6-year-old. Orthopedics. 1997;20:654–655.
- Morin O, Carlioz H. Osteoid osteoma of the floor of the ace tabulum in children: apropos of a case. Rev Chir Orthop Reparatrice Appar Mot. 1986;72:501–504.
- Motamedi D, Learch TJ, Ishimitsu DN, Motamedi K, Katz MD, Brien EW, Menendez L. Thermal ablation of osteoid osteoma: overview and step-by-step guide. Radiographics. 2009;29:2127– 2141.
- Mott MP, Meehan RE, Zhu H. Ilioinguinal approach to manage benign pelvic and acetabular tumors. Am J Orthop. 2001;30:554–
- 559.
- Mounach A, Nouijai A, Ghozlani I, Ghazi M, Achemlal L, Bezza A, El Maghraoui A. Osteoid osteoma of the acetabulum: a case report. Rheumatol Int. 2008;28:601–603.
- Mylona S, Patsoura S, Galani P, Karapostolakis G, Pomoni A, Thanos L. Osteoid osteomas in common and in technically challenging locations treated with computed tomagraphy-guided percutaneous radiofrequency ablation. Skeletal Radiol. 2010;39: 443–449.
- Norman A, Abdelwahab IF, Buyon J, Matzkin E. Osteoid oste oma of the hip stimulating an early onset of osteoarthritis. Radiology. 1986;158:417–420.
- Papagelopoulos PJ, Mavrogenis AF, Kyriakopoulos CK, Benetos IS, Kelekis NL, Andreou J, Soucacos PN. Radiofrequency abla tion of intraarticular osteoid osteoma of the hip. J Int Med Res. 2006;34:537–544.
- Parlier-Cuau C, Champsaur P, Nizard R, Hamze B, Laredo JD. Percutaneous removal of osteoid osteoma. Radiol Clin North Am. 1998;36:559–566.
- Philippon MJ, Schenker ML. Arthroscopy for the treatment of femoroacetabular impingement in the athlete. Clin Sports Med. 2006;25:299–308.
- Rosenthal DI, Hornicek FJ, Wolfe MW, Jennings LC, Gebhardt MC, Mankin HJ. Percutaneous radiofrequency coagulation of osteoid osteoma compared with operative treatment. J Bone Joint Surg Am. 1998;80:815–821.
- Rosenthal DI, Hornicek FJ, Torriani M, Gebhardt MC, Mankin HJ. Osteoid osteoma: percutaneous treatment with radiofre quency energy. Radiology. 2003;229:171–175.
- Rybak LD, Gangi A, Buy X, La Rocca Vieira R, Wittig J. Thermal ablation of spinal osteoid osteomas close to neural ele ments: technical considerations. AJR Am J Roentgenol. 2010;195: 293–298.
- Sampson TG. Complications of hip arthroscopy. Clin Sports Med. 2001;20:831–835.
- Sans N, Galy-Fourcade D, Assoun J, Jarlaud T, Chiavassa H, Bonnevialle P, Railhac N, Giron J, Morera-Maupome´ H, Railhac JJ. Osteoid osteoma: CT-guided percutaneous resection and fol lowup in 38 patients. Radiology. 1999;212:687–692.
- Simpson J, Sadri H, Villar R. Hip arthroscopy technique and complications. Orthop Traumatol Surg Res. 2010;96(8 suppl): S68–76.
- Sluga M, Windhager R, Pfeiffer M, Dominkus M, Kotz R. Peripheral osteoid osteoma: is there still a place for traditional surgery? J Bone Joint Surg Br. 2002;84:249–251.
- Smart LR, Oetgen M, Noonan B, Medvecky M. Beginning hip arthroscopy: indications, positioning, portals, basic techniques, and complications. Arthroscopy. 2007;23:1348–1353.
- Takaoka K, Yoshikawa H, Masuhara K, Sugano N, Ono K. Ectopic ossification associated with osteoid osteoma in the ace tabulum: a case report. Clin Orthop Relat Res. 1994;299:209–
- Tsurumoto T, Enomoto H, Shindo H. Intra-articular osteoid osteoma protruding from the acetabular fossa. Mod Rheumatol. 2005;15:286–289.
- Unni KK, Inwards CY. Osteoid osteoma. In: Unni KK, Inwards CY, eds. Dahlin’s Bone Tumors: General Aspects and Data on 10,165 Cases. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010:102–111.
- Vanderschueren GM, Taminiau AH, Obermann WR, Bloem JL. Osteoid osteoma: clinical results with thermocoagulation. Radiology. 2002;224:82–86.
- Ward WG, Eckardt JJ, Shayestehfar S, Mirra J, Grogan T, Oppenheim W. Osteoid osteoma diagnosis and management with low morbidity. Clin Orthop Relat Res. 1993;291:229–235.
- Yildiz Y, Bayrakci K, Altay M, Saglik Y. Osteoid osteoma: the results of surgical treatment. Int Orthop. 2001;25:119–122.
- Zampa V, Bargellini I, Ortori S, Faggioni L, Cioni R, Bartolozzi
